Heart Block
Basic Facts
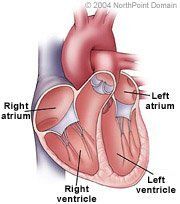
- Heart block, also called atrioventricular block or A-V block, is an abnormality of the spread or flow of electrical activity from the upper heart chambers, the atria, to the lower heart chambers, the ventricles.
- Heart block results in an abnormality or disturbance in the rate or rhythm of the heartbeat.
- Heart block occurs in three levels of severity. First-degree block is a delay of the signal that stimulates the ventricles to contract, and second-degree block is a partial or intermittent interruption of the signal that stimulates the ventricles to contract. Third-degree block is a complete interruption of the signal that stimulates the heart to contract.
Physicians classify heart block based on the length the delay: In first-degree heart block, the ECG shows one QRS wave for every P wave, but the pause is greater than normal. First-degree heart block: Heart beat impulses are delayed in the A-V node, but ultimately reach the ventricles. Sometimes, first-degree heart block can eventually lead to other forms of heart block.
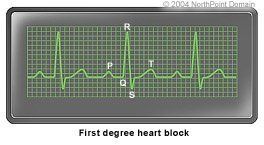
In first-degree heart block, the ECG shows one QRS wave for every P wave, but the pause is greater than normal.
Second-degree heart block: Heart beat impulses are delayed or blocked in or around the A-V node, and some of the impulses fail to reach the ventricles; Second-degree heart block is further divided into two sub-types:
- Type I second-degree heart block, also called Mobitz Type I heart block or the Wenckebach phenomenon.
- Type II second-degree heart block, also called Mobitz Type II block.
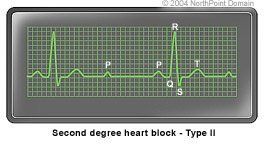
In second-degree type II block, notice that the P wave (4th bump) isn't followed by the QRS wave, because the ventricles weren't activated.
Third-degree heart block: Also called complete heart block, each sinus node impulse is completely interrupted in the A-V node or beyond, and the ventricles must generate their own impulse to contract. Depending on its cause, third-degree block may be transient (temporary) or permanent.
WHAT ARE THE SYMPTOMS?
Heart block symptoms can vary according to its type, frequency, duration, and whether underlying structural heart disease is present. Heart block can contribute to bradyarrhythmia, or an arrhythmia that causes an abnormally slow heart rate (fewer than 60 beats per minute). People with bradyarrhythmia may experience the following symptoms:
- Dizziness or lightheadedness;
- Low blood pressure;
- Palpitations (the sensation of skipped beats);
- Fatigue; and
- Syncope (fainting).
CAUSES AND RISK FACTORS
Heart block may occur at any age, but commonly becomes more frequent during middle age and is associated with aging. Among people without heart disease, the exact cause of heart block may be unknown. Milder forms of heart block may be caused by certain medications, including:
- Adenosine;
- Calcium channel blockers;
- Beta-blockers; and
- Digitalis.
- Endocarditis (inflammation of the tissue that lines the heart);
- Myocarditis (inflammation of heart muscle tissue);
- Lyme disease;
- Lenègre disease;
- Lev disease;
- Coronary heart disease; and
- Heart attack.
DIAGNOSIS
Because heart block may be unpredictable and brief, the condition can be difficult to diagnose. In addition to taking a person's medical history, listening to the patient describe symptoms, and conducting a physical examination, the physician will use one of the following tests: resting electrocardiogram, or ECG, or an ambulatory ECG using portable machines, either a Holter monitor or an event monitor.
TREATMENT APPROACH
A person's heart block may resolve naturally. In some cases, heart block may not be frequent, sustained, or bothersome enough to require treatment. Other forms of heart block can be controlled once the underlying heart disease. For example, in people who take a heart medication that may cause heart block, physicians may discontinue the use of the drug. When a person develops complete heart block following a heart attack, for example, the heart block may resolve with the healing of the area of heart muscle affected by the heart attack.
More severe forms of heart block that cause symptoms may require treatment, including pacing, which is the use of a pacemaker for electrical stimulation of the heart, and medication.
Common medications for heart block include atropine and isoproterenol. These drugs may be used in the short-term to treat a slow heart rate that causes symptoms, but second- and third-degree heart block may be unresponsive to atropine.
Copyright © 2017 NorthPoint Domain, Inc. All rights reserved.
This material cannot be reproduced in digital or printed form without the express consent of NorthPoint Domain, Inc. Unauthorized copying or distribution of NorthPoint Domain's Content is an infringement of the copyright holder's rights.
