Lower Extremity Disease
Basic Facts
- Lower extremity disease is a type of peripheral arterial disease. Lower extremity disease, also called leg artery disease, can prevent blood from reaching parts of the legs and feet.
- A common first symptom of leg artery disease is a discomfort in the legs during activity, called intermittent claudication. Intermittent claudication occurs with walking and running, and goes away when the activity has stopped.
- Eventually, lower extremity disease can cause sores on the legs, feet, and toes, known as ulcers, and even gangrene, or tissue death.
Lower extremity disease is a condition in which a medium to large artery that supplies oxygen-rich blood to the legs and feet becomes partially or completely blocked.
Lower extremity disease can be acute, meaning that it comes on quickly and ends. However, it is usually chronic, meaning it progresses slowly over a long period of time.
WHAT ARE THE SYMPTOMS?
Lower extremity disease usually develops over a long period, sometimes a decade or more. In most cases, there are no symptoms until a blockage in the artery or vein prevents more than half of the blood from passing through. Symptoms do not usually appear early in the disease.
As lower extremity disease progresses, symptoms may include:
- Pain, especially in the legs, calves, and buttocks;
- Blisters and ulcers on the skin that do not heal;
- Gangrene, or tissue death;
- Weak or absent pulse;
- Bruits (whooshing sounds a physician hears through a stethoscope);
- Muscle atrophy;
- Cooler skin temperature;
- Pale skin;
- Bluish or smooth and shiny, slowly growing nails; and
- Hair loss below the area of blockage.
CAUSES AND RISK FACTORS
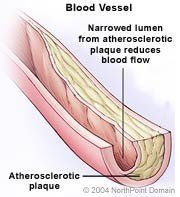
The main cause of lower extremity disease is atherosclerosis, or hardening of the arteries. As people age, plaque can build up inside their arteries. Over time, these plaques collect on arterial walls as cholesterol circulates in the blood. As the plaques enlarge, the arteries become narrow and stiff, resulting in atherosclerosis.
Factors that increase a person's risk for lower extremity disease include:
- Smoking;
- Advanced age;
- Male gender;
- Diabetes mellitus;
- High cholesterol; and
- High blood pressure.
DIAGNOSIS
If a physician suspects lower extremity disease based on a patient history and physical exam, he or she may order one or more of the following tests:
- Doppler flow velocity waveform analysis;
- Duplex ultrasound;
- Segmental pressure measurements;
- Magnetic resonance angiography, or MRA; and
- Contrast angiography.
TREATMENT APPROACH
Lower extremity disease is a serious condition. Left untreated, the disease will continue to progress and could cause gangrene, which could require amputation of the leg or the foot.
Physicians may prescribe medications for lower extremity disease including:
- Cilostazol;
- Pentoxifyllin;
- Platelet inhibitors;
- Thombolytic drugs; and
- Vascular endothelial growth factor.
Patients can control many risk factors for lower extremity disease, which can improve symptoms if a person has already been diagnosed. Physicians may order a special low-fat, low-cholesterol diet for a patient. If the medical condition permits, a physician will also recommend an exercise program. People with lower extremity disease must quit smoking.
When a patient with lower extremity disease has unrelenting pain or is in danger of losing a limb or becoming disabled, surgery may be necessary. Surgery may include:
- Bypass grafts;
- Synthetic grafts;
- Thromboendarterectomy;
- Sympathectomy;
- Amputation; or
- Angioplasty.
Copyright © 2017 NorthPoint Domain, Inc. All rights reserved.
This material cannot be reproduced in digital or printed form without the express consent of NorthPoint Domain, Inc. Unauthorized copying or distribution of NorthPoint Domain's Content is an infringement of the copyright holder's rights.
