Pericardial Disease
Basic Facts
- Pericardial disease refers to disorders involving the pericardium, the minimally fluid-filled, double-layered fibrous membrane that surrounds and protects the heart.
- Common types of pericardial disease include pericarditis, or inflammation of the pericardium, and pericardial effusion, or the accumulation of large amounts of fluid in the pericardium that compresses the heart muscle and causes other problems.
- Chest pain that accompanies pericarditis may be worsened by lying down, coughing, breathing deeply, and sometimes by swallowing.
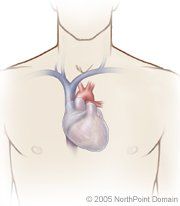
Pericardial disease is a disorder that involves the pericardium, the double-layered fibrous membrane surrounding the heart. Major disorders of the pericardium include:
- Acute pericarditis, inflammation of the pericardium;
- Cardiac tamponade, a rapid or large accumulation of fluid in the pericardial sac; and
- Chronic constrictive pericarditis, the persistence of pericarditis.
Both chronic and acute pericarditis can be life threatening. Therefore, if a person experiences any of the symptoms associated with pericardial disease, he or she should seek immediate medical attention.
WHAT ARE THE SYMPTOMS?
The most common symptoms of acute pericarditis are:
- Chest pain;
- Pericardial friction rub;
- Pericardial effusion;
- Dull chest pain; and
- Low-grade fever.
Symptoms of cardiac tamponade include:
- Severe drop in blood pressure;
- Rapid and difficult breathing;
- Weak pulse;
- Decreased heart sounds;
- Distended or bulging veins;
- Bluish skin color, or cyanosis; and
- Severe anxiety or panic.
People with chronic constrictive pericarditis commonly experience the following symptoms:
- Fatigue;
- Weakness;
- Shortness of breath;
- Weight loss;
- Loss of appetite;
- Liver enlargement;
- Distended neck veins;
- Ascites, or the accumulation of fluid in the abdomen; and
- Edema, or the accumulation of fluid in the extremities.
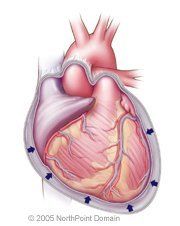
In cardiac tamponade, fluid builds up in the pericardium.
CAUSES AND RISK FACTORS
Acute pericarditis is often idiopathic, meaning it has no identifiable cause. The cause of chronic pericarditis is also often idiopathic, but it has been associated with the same conditions that cause acute pericarditis, which include:
- Bacterial, viral, or fungal infections;
- Autoimmune disorders;
- Cancer, especially Hodgkin's disease, and radiation treatment of cancer;
- Kidney failure;
- Side effects from drugs;
- Heart attack; and
- Heart surgery.
- Tumors;
- Uremia, or the accumulation in the blood of waste materials that are usually eliminated in the urine;
- Bleeding into the pericardium because of surgery or injury; and
- Bleeding caused by anticoagulants in patients with acute pericarditis.
DIAGNOSIS
In addition to taking a detailed medical history, listening to the patient describe symptoms, and performing a physical examination, the physician will order one or more of the following tests:
- Electrocardiography (ECG);
- Chest x ray;
- Blood tests;
- Echocardiography;
- A tuberculin skin test;
- Duplex ultrasonography;
- Computed tomography (CT) scan; and
- Magnetic resonance imaging (MRI).
Another technique a physician may use to diagnose the cause of pericarditis is pericardiocentesis, or the insertion of a needle through the chest wall or abdomen into the pericardium to remove fluid. The pericardial fluid is then analyzed to help determine the underlying cause of pericarditis.
TREATMENT APPROACH
The physician will treat acute pericarditis by prescribing medications, including:
- Nonsteroidal anti-inflammatories (NSAIDs), such as aspirin or ibuprofen;
- Morphine or codeine;
- Antiarrhytmic drugs;
- Antibiotics; and
- Corticosteroids.
If the underlying cause is viral, no further treatment is indicated and symptoms should clear in about a week.
If the fluid buildup is so great that the heart cannot pump effectively, the physician may perform pericardiocentesis. If the fluid re-accumulates, the physician may consider surgery to remove a portion of the pericardium so that fluid drains continuously.
Cardiac tamponade is a medical emergency and is treated by pericardiocentesis. To prevent fluid reaccumulation, a catheter is sometimes inserted into the pericardium and left in place for several days.
Several therapies may be used to reduce the accumulation of fluid in chronic constrictive pericarditis, including diuretics or abdominal paracentesis. Removal of the stiffened pericardium in a procedure called pericardiectomy is the only cure for chronic constrictive pericarditis.
Copyright © 2017 NorthPoint Domain, Inc. All rights reserved.
This material cannot be reproduced in digital or printed form without the express consent of NorthPoint Domain, Inc. Unauthorized copying or distribution of NorthPoint Domain's Content is an infringement of the copyright holder's rights.
