Pulmonary Embolism
Basic Facts
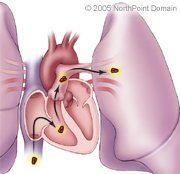
- The pulmonary arteries and their branches carry blood from the heart to the lungs to be oxygenated.
- A pulmonary embolism is the blockage or closure of a pulmonary artery or one of its branches by an abnormal object, most frequently a blood clot. The clot typically travels with the flow of blood from a leg vein to the site where it creates a blockage.
- When a pulmonary artery becomes severely blocked, blood oxygen levels fall, and blood pressure in the lungs and pulmonary arteries can rise so high that the heart may not be able to pump enough blood out of its chambers.
A pulmonary embolism occurs when an embolus, or abnormal object, moves through the circulatory system and blocks an artery in the lung. Because about 10 percent of pulmonary embolisms are fatal within the first hour after onset of symptoms, prompt diagnosis and treatment are critical.
If a blockage occurs in a large blood vessel or if the person suffers from another pulmonary condition, such as pulmonary hypertension, the blockage could cause pulmonary infarction, which means lung tissue death.
WHAT ARE THE SYMPTOMS?
The severity of the symptoms varies with the size or number of blockages. Small embolisms may cause no symptoms. Common symptoms include:
- Shortness of breath;
- Chest pain, sometimes radiating into the shoulder, arm, neck, and jaw;
- Rapid breathing;
- Anxiety and restlessness;
- Lightheadedness;
- Rapid heartbeat;
- Syncope, or fainting;
- Pleural friction rub, which is a rubbing sound in the chest;
- Weak pulse;
- Low blood pressure;
- Coughing or spitting up blood;
- Bluish skin tone (cyanosis); and
- Wheezing.
CAUSES AND RISK FACTORS
About 50 percent of all embolisms are blood clots that result from a condition called deep vein thrombosis (DVT). Rarely, a pulmonary embolism can be caused by an air bubble, fat, amniotic fluid (in mothers shortly after childbirth), or bone marrow following a fracture.
The following factors increase a person's risk for a pulmonary embolism.
- Family history;
- Blood clotting disorders;
- Major surgery;
- Prolonged immobility;
- Cancer;
- Prior embolism;
- Obesity;
- Heart conditions;
- Smoking;
- High blood pressure;
- Use of birth control pills;
- Hormone replacement therapy (HRT);
- Pregnancy and childbirth;
- Advanced age; and
- Pelvis, hip, or leg fractures.
DIAGNOSIS
A physician will take a patient's history and will order one or more of the following tests:
- Chest x ray;
- Electrocardiography (ECG);
- D-dimer Enzyme-Linked Immunosorbent Assay (ELISA);
- Lung ventilation scanning;
- Computed tomography (CT) scan;
- Contrast pulmonary angiography; or
- Duplex ultrasonography.
TREATMENT APPROACH
The mainstay of treatment for pulmonary embolism is the anticlotting drug heparin, which is usually given intravenously.
Patients may also receive analgesics (pain-killers), oxygen, or drugs that stabilize blood pressure level and heart rhythm.
In patients who experience a massive pulmonary embolism and who have a pre-existing heart condition or other health problem, the physician may use more aggressive treatments. One option is thrombolysis, or the administration of thrombolytic (often called clot-busting) drugs. Because anticlotting drugs increase the risk of severe bleeding, patients receiving them are carefully monitored. A pulmonary embolectomy, surgery to remove a life-threatening embolism, may also be indicated in very severe cases.
Once a pulmonary embolism has been effectively treated, patients are usually given a blood-thinning drug such as warfarin (trade name Coumadin). Most patients require blood-thinning medication for at least 6 months. Because these drugs can make a patient prone to excessive bleeding, patients are regularly given blood tests to check how long it takes the blood to clot.
A patient who develops recurrent pulmonary embolisms despite drug therapy may be treated with a device known as an inferior vena cava filter, a device that is designed to capture clots near their origin in the bloodstream.
LIFESTYLE
Patients with a known risk of pulmonary embolism can adopt several lifestyle measures to reduce the chances of developing a blood clot, including:
- Wearing compression stockings daily;
- Receiving a treatment called intermittent pneumatic compression;
- Moving around every hour during long car rides and plane trips;
- Taking a low dose of aspirin during long trips (if not already taking blood-thinners); and
- Drinking plenty of fluids.
Copyright © 2017 NorthPoint Domain, Inc. All rights reserved.
This material cannot be reproduced in digital or printed form without the express consent of NorthPoint Domain, Inc. Unauthorized copying or distribution of NorthPoint Domain's Content is an infringement of the copyright holder's rights.
