Sleep Apnea
Basic Facts
- Sleep apnea is a condition in which people experience multiple episodes of apnea (stop breathing repeatedly, usually for at least 10 seconds) during sleep, which disturbs the sleep-wake cycle.
- Over an 8-hour sleep period, a person can experience hundreds of apneic episodes.
- People who have this condition are at increased risk for cardiovascular disease.
- Treatment for sleep apnea includes lifestyle changes, use of mechanical devices, and surgery.
Sleep apnea is a condition in which people experience multiple episodes of apnea (stop breathing repeatedly, usually for at least 10 seconds) during sleep, which increases a person's risk for numerous cardiovascular conditions. The body reacts to this interruption in breathing by forcing the body to inhale, which partially awakens the patient. The patient does not typically fully wake up, but apneic events are enough to disturb the sleep cycle, resulting in poor sleep quality. Apneas can occur 20 to 60 times per hour. Over an 8-hour sleep period, a person can experience hundreds of apneas. Sleep apnea is common, and an estimated 12 million Americans have the condition.
There are 2 types of sleep apnea:
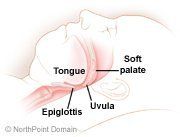
- Obstructive sleep apnea: Tissue in the upper airway completely or partially collapses intermittently during sleep and blocks or obstructs the airway.
- Central sleep apnea: The brain fails to signal the respiratory muscles to breathe, causing the oxygen levels in the blood to decrease rapidly.
Symptoms of both types of sleep apnea include:
- Snoring, coughing, snorting, or gasping for breath during sleep;
- Daytime sleepiness;
- Morning headaches;
- Forgetfulness;
- Depressed mood;
- Decreased interest in pleasurable activities, such as sex; and
- Drowsiness while driving.
Risk factors for OSA include:
- Acromegaly;
- African American, Pacific islander, or Mexican descent;
- Age older than 40 years;
- Alcohol use;
- Amyloidosis;
- A narrow upper airway;
- Diabetes mellitus;
- Enlarged tonsils, adenoids, and/or tongue;
- Family history of sleep apnea;
- Gastroesophageal reflux disease;
- Hypothyroidism;
- Male gender;
- Neurological conditions that impair upper respiratory muscle tone;
- Obesity;
- Polycystic ovarian syndrome;
- Polyps in the upper airway;
- Recessed chin; and
- Smoking.
Factors that increase a person's risk for central sleep apnea include central nervous system disorders such as stroke and encephalitis and neuromuscular disorders like amyotrophic lateral sclerosis (Lou Gehrig's disease).
Certain drugs can worsen sleep apnea, including alcohol, anti-anxiety medications, antihistamines, sedatives, and other central nervous system depressants.
Treatments for sleep apnea include lifestyle changes, mechanical therapy, and surgical approaches.
WHAT CONDITIONS WILL IT HELP?
Untreated sleep apnea increases a person's risk for developing and worsens the following conditions:
- Hypertension;
- Arrhythmias;
- Pulmonary hypertension;
- Heart failure;
- Acute myocardial infarction; and
- Stroke.
People with untreated sleep apnea are at increased risk for morning headaches, memory problems, depressed feelings, gastroesophageal reflux, erectile dysfunction, poor job and academic performance, and motor vehicle accidents.
GETTING STARTED
People who suspect that they have sleep apnea can take a test, which determines their "snore score."
WHAT TO EXPECT
Tests the physician uses to diagnose sleep apnea include:
- Oximetry (records and monitors the oxygen level in the patient's blood);
- Polysomnography (records a variety of body functions during sleep, such as the electrical activity of the brain, eye movement, muscle activity, heart rate, respiratory effort, airflow, and blood oxygen levels); and
- The Multiple Sleep Latency Test (MSLT) (measures how quickly a patient falls asleep).
Treatment of sleep apnea, which is typically tailored to the individual patient and depends on the severity of the apneic events, includes lifestyle changes, medication, devices, and surgical intervention.
Lifestyle changes include:
- Losing weight if necessary;
- Avoiding avoid alcohol, antihistamines, sleep aids, and sedatives;
- Changing sleeping positions from the back to the stomach or side; and
- Practicing good sleep habits.
Devices used to treat sleep apnea include:
- Nasal continuous positive airway pressure (CPAP) (patient wears a mask over the nose during sleep, which is connected to a hose, which is connected to an electric air pump. The pump sends air through the hose, and the air pressure moving through the hose and mask forces air through the nasal passages, keeping the airway open); and
- Dental appliances (reposition the lower jaw and the tongue).
Surgical procedures used to treat sleep apnea include:
- Uvulopalatopharyngoplasty (removing excess tissue at the back of the throat);
- Laser-assisted uvulopalatoplasty (using a laser device to eliminate tissue in the back of the throat);
- Somnoplasty (uses radio waves to reduce the size of some airway tissue, such as the uvula and the back of the tongue); and
- Other procedures (surgical reconstruction of the lower jaw, tracheostomy, or obesity surgery).
HOW SOON WILL IT MAKE A DIFFERENCE?
Some lifestyle changes can make a difference almost immediately as can devices such as CPAP and surgical procedures. Other lifestyle changes, such as weight loss, may take weeks or months before the patient notices improvement.
Copyright © 2017 NorthPoint Domain, Inc. All rights reserved.
This material cannot be reproduced in digital or printed form without the express consent of NorthPoint Domain, Inc. Unauthorized copying or distribution of NorthPoint Domain's Content is an infringement of the copyright holder's rights.
