Syncope
Basic Facts
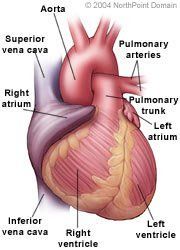
- Syncope (fainting) is a sudden temporary loss of consciousness, which results when the heart does not pump enough oxygenated blood to the brain.
- Syncope can have many causes that can range from benign to life-threatening.
- Heart disease, including blocked coronary arteries, arrhythmias, and congestive heart failure, can cause syncope.
- Treatment for syncope focuses on identifying and treating the underlying cause for the syncope.
Syncope, or fainting, is a sudden loss of consciousness with a rapid, spontaneous recovery.
Syncope often recurs and it can be harmless to life threatening. Therefore, people who experience an episode of syncope should seek medical attention.
Physicians group syncope into three categories:
- Noncardiac syncope;
- Cardiac syncope; and
- Syncope of unknown cause.
Most commonly, syncope does not occur because of a heart condition. Cardiac syncope results from arrhythmias or a disorder that reduces the heart's ability to pump enough blood to meet the body's needs. Treatments for syncope depend on its cause and can include adjusting medications, taking medications, pacemaker implantation, and surgical procedures.
WHAT ARE THE SYMPTOMS?
Syncope often occurs without any symptoms. Symptoms can include:
- Sweating;
- Dizziness;
- Weakness;
- Nausea; and
- Pallor.
CAUSES AND RISK FACTORS
Causes of noncardiac syncope include:
- Malfunction of the body's blood pressure regulation system;
- Being in a crowded area;
- Being in a warm area;
- Emotional stress;
- Pain;
- Dehydration;
- Rising suddenly from a prone position;
- Vigorously coughing, swallowing, or straining to defecate;
- Narrowed carotid arteries;
- A stroke or transient ischemic attack;
- Diabetes mellitus;
- Autonomic nervous system disorders such as a spinal cord injury; and
- Medications such as antihypertensives, antidepressants, or Parkinson's drugs.
Cardiac syncope is caused by arrhythmias and conditions that can reduce the amount of blood the heart pumps, including:
- Sick sinus syndrome;
- Heart block;
- Supraventricular tachycardia;
- Ventricular tachycardia;
- Ventricular fibrillation;
- Valve disorders;
- Hypertrophic cardiomyopathy;
- Pulmonary embolism;
- Certain congenital heart disorders;
- Myocardial ischemia;
- Pulmonary hypertension; and
- Congestive heart failure.
Syncope can also be a symptom of a malfunctioning man-made replacement heart valve or a malfunctioning pacemaker.
Factors that increase a person's risk for syncope include female gender and age.
DIAGNOSIS
The physician will perform a detailed medical history and a physical examination.
The physician may also order the following tests:
- Electrocardiogram (ECG);
- Tilt table testing;
- Electroencephalography;
- Electrolyte levels;
- ECG stress test;
- Ambulatory ECG;
- Electrophysiology testing;
- Echocardiography; and
- Cardiac catheterization and angiography.
TREATMENT APPROACH
Treatment of syncope depends on its cause.
Patients with syncope should consult with their physicians regarding potentially dangerous activities, such as driving, certain jobs, or recreational activities.
Immediate treatment for most forms of noncardiac syncope includes having the person lie horizontally to restore consciousness. Treatment to prevent recurrent noncardiac syncope includes:
- Education; and
- Adjusting or prescribing medications
Treatment of cardiac syncope is based on addressing the underlying cardiac condition and includes:
- Medications;
- Implantable cardioverter defibrillator (ICD);
- Pacemaker;
- Radiofrequency catheter ablation;
- Valvular surgery;
- Coronary artery bypass graft surgery;
- Angioplasty and stenting; and
- Congenital heart surgery.
Copyright © 2017 NorthPoint Domain, Inc. All rights reserved.
This material cannot be reproduced in digital or printed form without the express consent of NorthPoint Domain, Inc. Unauthorized copying or distribution of NorthPoint Domain's Content is an infringement of the copyright holder's rights.
